Migraine With Comorbid Depression: Pathogenesis, Clinical Implications, and Treatment
Migraine is a neurological disorder that strongly relates to psychiatric conditions like depression. Lately, the increased prevalence of depression in migraineurs has come to attention. This article compiled various literature to explore the association between migraine and depression. Genetic overlap of various gene segments was studied, and heritability patterns were explored.
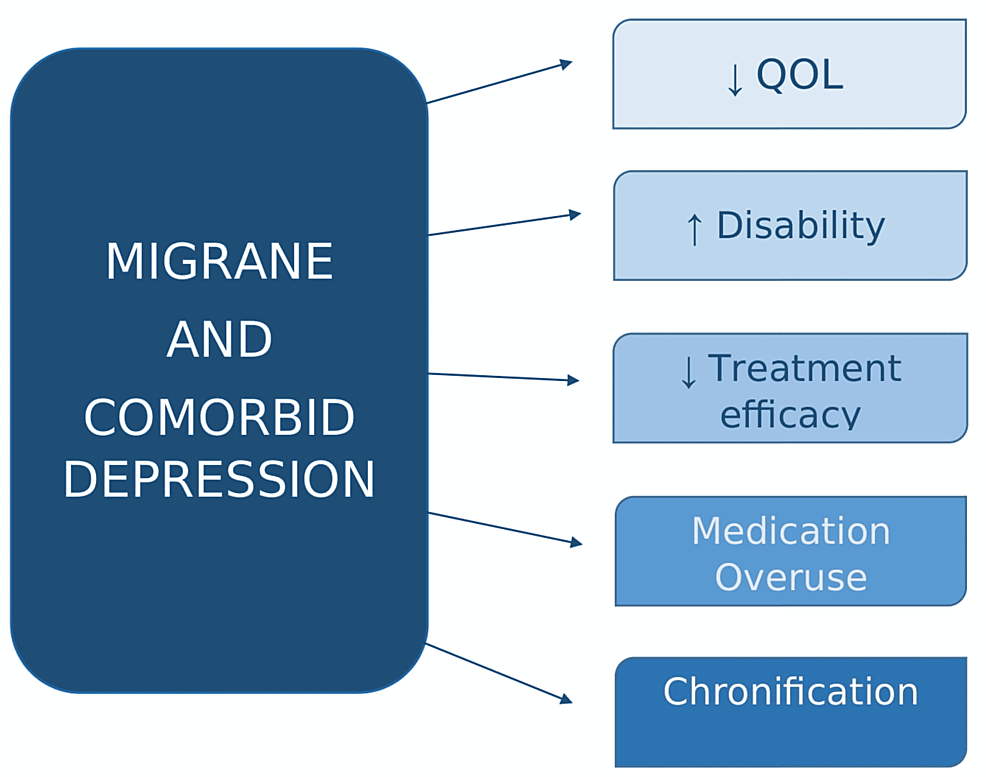
Conclusion/Relevance: Migraine with comorbid depression (MID) affects various aspects of life and its clinical impact on migraine disability, quality of life (QOL), progression, and medication overuse was investigated. We further inspected several types of research in order to provide options on various treatment modalities. Pharmacotherapy such as antidepressants and anti-Calcitonin Gene-Related Peptide (CGRP) monoclonal antibodies like fremanezumab were studied. Alternative treatment options such as onabotulinumtoxinA (OBTA) injections, cognitive behavioral therapy (CBT), and vagal nerve stimulations (VNS) were also appraised and the efficacies of each were compared.

• Source: Cureus
• Relevance: “Migraine is a neurological disorder that strongly relates to psychiatric conditions like depression. Lately, the increased prevalence of depression in migraineurs has come to attention. This article compiled various literature to explore the association between migraine and depression.”
• Depression is often a comorbidity of migraine, which could be due to shared factors such as heritability, serotonergic dysfunction, genetic overlap, environmental stressors, structural brain changes, and MTHFR polymorphism.
• Individuals with depression and migraine exhibit increased headache days, worse quality of life, and higher disability vs. those with migraine alone.
• “Efficient management of MID [migraine with comorbid depression] becomes imperative, given its impact on the clinical course and progression. For that purpose, the commonalities between migraine and depression were targeted, such as the use of antidepressants to treat both simultaneously. Several alternative drugs and treatment methods have been sought to answer this conundrum,” the authors write.
• The authors discuss alternative treatments including cognitive-behavioral therapy (CBT), vagus-nerve stimulation, OnabotulinumtoxinA, and monoclonal antibodies.
• The authors state, “So far, only this one study has been done to evaluate fremanezumab in MID. However, encouraged by the results, at least one more is currently ongoing. Similarly, another CGRP monoclonal antibody, galcanezumab, has shown some effectiveness in MID.”